One of the most enduring myths in modern medicine is that high cholesterol levels cause heart disease. You might find it surprising, therefore, that study after study has failed to prove any link between blood cholesterol levels and artherosclerosis.
Abundant evidence that the cholesterol theory is wrong.
This was known as far back as 1936 when K Lande and W Sperry examined the bodies of 123 recently deceased people and found absolutely no correlation between the cholesterol blood levels and lipid levels in the aorta. In a 1960 study, JC Paterson examined the levels of atherosclerosis in 191 deceased veterans and concluded -
‘The complications of atherosclerosis were just as frequent in cases with low serum cholesterol levels.’
The authors of a 1973 study published in the British Heart Journal examined 71patients and concluded -
‘In this study, we failed to confirm any relation between the degree of obstructive lesions verified angiographically and blood lipid levels.’
A paper published in the British Medical Journal in 2016 also failed to find any evidence that high cholesterol in elderly patients had any correlation with cardiovascular mortality. In fact, they found the opposite – people over 60 with high levels of cholesterol had a lower risk of dying than those with lower cholesterol.
The authors stated –
“High LDL-C is inversely associated with mortality in most people over 60 years. This finding is inconsistent with the cholesterol hypothesis (i.e., that cholesterol, particularly LDL-C, is inherently atherogenic).”
A 2003 study of elderly patients in hospitals also found cholesterol levels were inversely related to mortality rates as did a Finnish study who examined the link between cholesterol levels and mortality in the elderly.
One trial, based on the drug Evacetrapib, was supposed to highlight the benefit of raising HDL (the good cholesterol) whilst also lowering LDL (bad cholesterol). LDL was reduced by 37% but there was no positive outcomes at all for the patients. In 2008, it was reported that another two drugs that were proven to lower cholesterol had no impact on heat attacks.
A recent report in the British Medical Journal even admitted that, after examining 35 trails, they found no evidence that reducing cholesterol levels have led to any benefit to patients and are now questioning the Cholesterol hypothesis.
” Considering that dozens of [randomised controlled trials] of LDL-cholesterol reduction have failed to demonstrate a consistent benefit, we should question the validity of this theory.”
They concluded - “In most fields of science the existence of contradictory evidence usually leads to a paradigm shift or modification of the theory in question, but in this case the contradictory evidence has been largely ignored, simply because it doesn’t fit the prevailing paradigm.”
So many papers have been written that disprove the cholesterol theory and, in fact, show that low cholesterol levels are dangerous, that author David Evans has collated them into a book entitled, “Low Cholesterol Leads to an Early Death. Evidence from 101 scientific papers.”

With all the evidence against the cholesterol theory, what data do the proponents of it cite to bolster their case?
The dubious evidence of the pro-cholesterol theory proponents.
One of the studies proponents of the cholesterol theory quote is the Framingham Study. This 1950s study involved measuring the blood serum cholesterol levels in 1959 men and 2415 women and seeing if there was any correlation to cardiovascular disease. The advocates of the cholesterol theory claim that the study proved that a 1% reduction in cholesterol corresponded to a 2% reduction in in CVD risk. Here, however, is a quote from a 1987 paper that followed the progress of the participants in the study –
“There is a direct association between falling cholesterol levels over the first 14 years and mortality over the following 18 years (11% overall and 14% CVD death rate increase per 1 mg/dL per year drop in cholesterol levels).”
In other words, as the participants’ cholesterol decreased their risk of dying of any disease increased as did their risk of dying from heart disease. However, in the same paper they claim that for people under 50 there is a higher risk of dying with high cholesterol for a period of 30 years but no association whatsoever between cholesterol levels and mortality if over 50! So apparently if you can survive the higher risk of low cholesterol for 14 years and you are under 50, lower cholesterol will then mysteriously be beneficial rather than detrimental until you reach 50 when cholesterol won’t matter at all. This, apparently, is medical science.
The other study is the infamous 1958 Seven Countries study conducted by the American physiologist, Ancel Keys. However, Keys was accused of selective use of data when he conducted the study, which was supposed to prove that high fat intake and therefore, high cholesterol levels, led to increased incidences of heart disease.
Statistician, Russell H Smith, examined the study and said –
“The dietary assessment and methodology was highly inconsistent across cohorts and thoroughly suspect. In addition, careful examination of the death rates and associations between diet and death rates reveal a massive set of inconsistencies and contradictions.”
He went on to say –
“In summary, the diet CHD (coronary heart disease) reported for the Seven Countries Study cannot be taken seriously by the objective scientist.”
The accusation of being selective in his use of data was also levelled at Keys in his previous 1953 paper, “Artherosclerosis: A problem in New Public Health.” In this study he collated data from 22 countries but only chose the information from six that seemed to prove his theory, disregarding the other data sets. In fact, critics of the study highlighted the lack of scientific rigour when they chose their own list of data sets from those that Keys rejected and proved an inverse relationship between fat intake and cardiovascular disease.
In 1977, Keys admitted that –
“There’s no connection whatsoever between cholesterol in food and cholesterol in the blood. And we’ve known that all along.”
This because cholesterol in the diet makes up only 20% of overall cholesterol level, because the vast majority of cholesterol is manufactured in the liver, which regulates the amount in body, keeping the total amount in balance.
Why the body needs Cholesterol.
The much-maligned cholesterol is actually essential for optimum health. It is needed to produce vitamin D, sex hormones and bile salts. It is also essential for the integrity of all the cells in your body and is also an integral part of the myelin sheath that protects each neuron. It is also a vital part of the body’s ability to repair damaged blood cells. Almost 25% of all cholesterol is in the brain, where it is essential for proper cognitive functioning.
Cholesterol and vitamin D
Cholesterol is essential for the production of vitamin D. Low levels of cholesterol should therefore adversely impact vitamin D production. It is interesting that vitamin D deficiency is known to be linked to various cardiovascular problems. Therefore, it follows, that low rather than high cholesterol levels could lead to heart issues.
Vitamin D is also is also essential for the immune system as it helps protect against viral and bacterial infection. It is no coincidence, therefore, that high levels of blood serum cholesterol are also known to protect against many infectious diseases including urinary tract infections and musculoskeletal and skin infections. According to an article in the International Journal of Medicine, after a meta-analysis of 19 different studies, it was shown that there was an inverse relationship between cholesterol levels and mortality from respiratory, gastrointestinal diseases and Aids.
Cholesterol and bile salts
Bile salts are produced in the liver and are derived from cholesterol. Their function in the digestive process is to break down fats for absorption. Any disruption to the bile salt production process can lead to digestive problems such as Irritable Bowel Disease and impaired biosynthesis from cholesterol is a factor in the disease. Adequate cholesterol levels are important as IBD sufferers have been shown to have low levels.
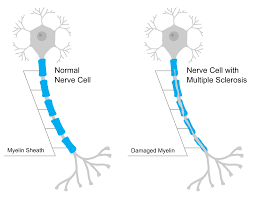
Cholesterol and the Myelin Sheath
Cholesterol is a major component of the myelin sheath. It is the destruction of the myelin that leads to neurodegenerative diseases such as multiple sclerosis. Cholesterol plays a crucial role in repairing the damage to myelin, so low levels of cholesterol, or any alteration in the production of cholesterol, exacerbates the disease.
Cholesterol and Dementia
As cholesterol is an essential component of brain cells, it should be expected that high levels may be a protective factor against cognitive decline. This is exactly what the authors of a paper in the journal, ‘Neurology’ discovered. They found that high cholesterol levels reduced the risk of dementia for people aged 79 to 88.
As noted, any disruption the cholesterol production process can lead to damage to the myelin sheath. It has now been discovered that insufficient nerve insulation, due to a lack of myelin, can lead to Alzheimer’s. A study examined the effect of variations in a gene which regulates cholesterol transport to the brain. The authors of the study found that myelin sheaths tended to be fewer and thinner in brains that carried the variant that caused cholesterol transport to be reduced, which substantially raised the risk of dementia.
These two studies emphasise the importance of sufficient levels of cholesterol for proper cognitive functioning.
If it’s not cholesterol, what are the possible causes of artherosclerosis?
According to the cholesterol theory of heart disease LDL (Low Density Lipoprotein) cholesterol is bad and HDL (High Density Lipoprotein is good). The former is considered bad because it delivers cholesterol to the arteries, where it sometimes accumulates in damaged blood vessels. HDL is good because it removes excess cholesterol and returns it to the liver. However, both LDL and HDL are doing exactly what they are designed to do. LDL transports cholesterol to the cells that need it and HDL removes excess cholesterol. Neither is bad nor good.
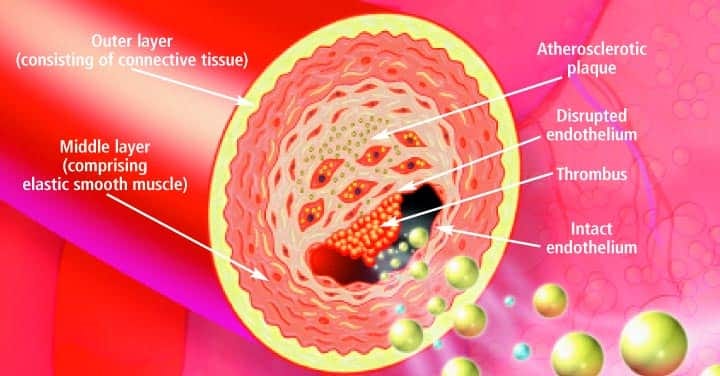
LDL is not the cause of atherosclerosis. For cholesterol to accumulate in the arteries they need to be damaged first. As is frequently the case, the medical profession mistakes a symptom for a cause. The first step in atherosclerosis is endothelium dysfunction and this is caused by a depletion of nitric oxide leading to the blood vessel’s reduced ability to dilate properly.
Nitric Oxide also inhibits other processes which are steps in the pathway to artherosclerosis. It “inhibits platelet aggregation, prevents adhesion of platelets to the endothelial surface and induces disaggregation of aggregating platelets. It inhibits the activation and expression of certain adhesion molecules and modulates adhesion of white cells to the vessel wall. Smooth muscle cell replication and migration are also inhibited by NO”
So, what conditions cause depletion in nitric oxide levels and are known risk factors for heart disease.?
Raised Homocysteine Levels
Homocysteine is an amino acid that is required for protein synthesis. An excess of it, however, is toxic and can lead to numerous health problems, including heart disease. High levels cause oxidative stress which impairs the functioning of the endothelial cells of the arteries, leading to thrombosis. Other mechanisms involved are due to high homocysteine levels’ ability to cause inflammation and promote cell death as well as interfere with nitric oxide production which is necessary for the dilation of blood vessels.
The link between the amino acid and heart disease was discovered in the 1960s by a Dr Kilmer McCully but, over the following years, with the cholesterol theory becoming the general consensus, his work was ignored. Recently, however, due to the ever-mounting evidence, excess homocysteine is now accepted as a risk factor.
An article in the Nutrition Journal states-
“There has been an indication towards a significant correlation between hyperhomocysteinemia and cardiovascular disease and its complications such as heart attacks and strokes.”
It goes on to say –
“Homocysteine has been recognized as a risk factor as early as 1990s, for the presence of atherosclerotic vascular disease and hypercoagulability states. “
It has also been demonstrated that vitamin D levels are inversely associated with homocysteine levels. As previously noted, low vitamin D can be a factor in cardiovascular problems so this may be one of the mechanisms involved.
So, how are high homocysteine levels rectified? By simply ensuring one has enough vitamins B6, B12 and folic acid.
Stress
Everyone knows that if you have a heart problem you should try to avoid stress. So how are stress and heart attacks related?
The stress response releases cortisol from the adrenal glands which narrows the arteries and epinephrine makes the heart work faster and raises blood pressure in preparation for the’ fight or flight ‘response. This is fine as long as the stress is short-lived but, if it persists, it can lead to serious health issues including heart problems.
A study involving 861 patients was published in 2010 which concluded –
“High cortisol levels strongly predict cardiovascular death among persons both with and without preexisting cardiovascular disease. The specific link with cardiovascular mortality, and not other causes of mortality, suggests that high cortisol levels might be particularly damaging to the cardiovascular system.”
Another study found that every time a combination of stress hormones doubled, there was 21 to 31% increase in the risk of hypertension, a known cause of heart attacks, and 90% increased risk of cardiovascular events with each doubling of cortisol levels.
One of the mechanisms involved in stress-induced heart disease is the reduction in nitric oxide, which, as previously discussed, results in endothelial dysfunction and the progression of atherosclerotic plaques.
According to an article in Frontiers in Cardiovascular Medicine –
“It was found that under chronic stress, thoracic aortic rings exhibited high sensitivity to vasoconstrictors by inhibiting nitric oxide synthase activity or removing endothelial cells. Chronic stress could reduce NO production and induce physiological and biological changes of blood vessels, leading to endothelial dysfunction and the progression of atherosclerotic plaques.”
Vitamin C Deficiency
Vitamin C has been shown to increase production of nitric oxide in the endothelium, thus promoting better vasodilation.
A metanalysis of 44 trials showed that short-term supplementation with vitamin C was found to reduce endothelial dysfunction in subjects with with heart failure and atherosclerosis. Numerous other studies have shown an inverse relationship between vitamin C levels and coronary heart disease. The vitamin has also shown to promote endothelial cell proliferation, inhibit apoptosis and tighten the endothelial permeability barrier, all of which lead to better blood vessel integrity and, therefore, less chance of endothelial dysfunction.
The Dangers of Statins
The main drugs prescribed to lower cholesterol are statins. They do this by inhibiting the enzyme HMG-CoA reductase (HMGCR), which regulates the production of cholesterol in the liver. Unfortunately, as noted, cholesterol is not the cause of atherosclerosis and so reducing it does not prevent the disease nor alleviate its symptoms. Statins do, however, cause serious health issues such as Statin-Associated Muscle Symptoms (SAMS), type 2 diabetes mellitus, neurological and neurocognitive effects, hepatotoxicity, renal toxicity.
The term Statin-Associated Muscle Symptoms sounds like a relatively mild condition but it covers illness such as rhabdomyolysis which involves severe muscle pain due to the disintegration of muscle tissue which in turn can lead to renal damage as fragments of muscle tissue enter the blood stream and end up in the kidneys. The very first statin, cerivastatin, was withdrawn from the market in 2001 due to 52 deaths due to statin-induced rhabdomyolysis. SAMS can also include the even more devastating disease necrotizing myositis, commonly known as flesh-eating disease, which can have a fatality rate of up to 80%. In statins patients it is caused by autoantibodies to the HMG-CoA reductase enzyme that the statins target.
Moreover, the medical profession admits that necrotizing myositis is hard to diagnose and have no idea how to treat it as this statement from the Autoimmune Reviews journal makes clear -
“Statin-induced autoimmune myositis remains a rare (and likely new) subset of the statin-induced myopathy spectrum. As such, presentation, response to treatment and long-term prognosis remain incompletely defined and the evidence base for best-practice treatment is lacking.”
Interfering with the function of the HMGCR has other consequences. According to an article in the Journal of Lipid research, when the HMG-CoA reductase enzyme was de-activated in mice they ‘developed hepatic steatosis with apoptosis, hypoglycemia, and eventually liver failure and death.’ In another animal model, the inhibition of HMGCR resulted in brain haemorrhaging. The study, mentioned in Developmental Biology, states-
“Inhibition of HMGCR function perturbs cerebral-vascular stability, resulting in progressive dilation of blood vessels, followed by vessel rupture, mimicking cerebral cavernous malformation (CCM)-like lesions in humans and murine models.”
The Importance of the Mevalonate Pathway.
Blocking the HMGCR enzyme does not just hinder the production of cholesterol, it interferes with many other important processes. HMGCR catalyses the conversion of HMG-CoA to mevalonic acid, the first step along then Mevalonate pathway. The pathway leads to the production of organic compounds called isoprenoids, so inhibiting HMGCR also hinders the production of these.

Dolichols
Dolichols are essential isoprenoids for the process known as N-linked glycosylation, whereby a carbohydrate is attached to a protein molecule. This in turn is required for the proper formation of proteins or protein folding. If there is any disruption to this process it can result in malformed or unfolded proteins. If too many of these accumulate in the body, the Unfolded Protein Response is activated which can lead to cell death. Diseases that can result from the activation of the UPR in the liver are obesity-associated fatty liver disease, viral hepatitis, and alcohol-induced liver injury.
However, if auto-antibodies to the enzyme are formed, as in the case with necrotising myotis, then the body’s immune system will attack them throughout the body and this could lead to a system-wide UPR response as detailed in an article in the journal, ‘Brain Pathology.’ This could result in illnesses other than just necrotizing myositis such as amyotrophic lateral sclerosis, Parkinson’s disease, Huntington’s disease, Alzheimer’s disease, multiple sclerosis, Pelizaeus-Merzbacher disease, and transverse myelitis. It can also lead to prion-related disorders, the most well-known of which is Creutzfeldt-Jakob disease (the human equivalent of mad cow disease).
A pharmacovigilance study based on the FDA Adverse Events Reporting Scheme has actually listed cases of prion disorders and Creutzfeldt Jacob diseases caused by statins as well as numerous cases of other neurocognitive disorders caused by the drugs.
Ubiquinone
Another isoprenoid disrupted by the inhibition of the HMGcoA reductase enzyme is ubiquinone. Ubiquinone, commonly known as coenzyme Q10, is a major antioxidant and important for the optimal functioning of mitochondria – the energy powerhouses of the cells – as it is necessary for the production of adenosine triphosphate.
Co-Q10 deficiency can lead to a wide spectrum of illness including encephalomyopathies with recurrent myoglobinuria, cerebellar ataxia, heart failure, Parkinson's disease, and malignancy. Myoglobinuria is similar to rhabdomyolysis and can result in kidney failure and cardiac arrest. Cerebellar ataxia leads to the inability to control muscle movements in the limbs and impairment of speech.
So, a drug created to reduce heart attacks can actually cause them because it disrupts the production of Co-Q10. In fact, supplementation with Co-Q10 has shown to improve various parameters associated with congestive heart failure, highlighting its importance for good cardiovascular health.
Selenoproteins
Another way in which statins can cause heart problems is due to the effect they have on selenoproteins which are also created via the mevalonate pathway. The Indian Journal of Endocrinology and Metabolism states the following -
“Statins reduces the availability of isopentenylpyrophosphate, leading to a decrease in production of selenoproteins. Selenium deficiency caused myopathy and cardiomyopathy resembling statin-induced myopathy.”
The journal also admits that low cholesterol can exacerbate heart problems -
“Some reports noted harmful effects of statins in patient with cardiac failure since it was observed that low cholesterol is associated with poor outcome in such patients.”
Heme
One other effect of inhibiting the HMGCoA reductase enzyme, and the mevalonate pathway, is the disruption to the production of heme. Heme binds oxygen in the blood and is necessary for the synthesis of nitric oxide production and essential for various cardiovascular processes.
A study in, ‘Expert review of Clinical Pharmacology’, has shown that statins promote endothelial dysfunction, the actual cause of atherosclerosis. The reasons the authors of the study cite for this, is due to the drug reducing the production heme, co-enzyme Q10 and the impairment to the selenoproteins synthesis process. They conclude by stating –
“Thus, the epidemic of heart failure and atherosclerosis that plagues the modern world may paradoxically be aggravated by the pervasive use of statin drugs. We propose that current statin treatment guidelines be critically reevaluated.”
Another study also states that statins cause endothelial dysfunction –
“Increased statin dosage may induce MD (mitochondrial dysfunction) and contribute to endothelial dysfunction in patients with CAD (coronary artery disease).
The Package Insert Data
Irrespective of studies, numerous possible side effects are listed on the actual data sheet that accompanies the drug. The one with Lovastatin includes eye damage, facial paralysis, anxiety, depression, psychic disturbances, memory loss, arthritis, anorexia, angioedema, thrombocytopenia, and the even more dangerous conditions such as hepatic failure, lung disease, lupus, pancreatitis, hepatitis, Stevens-Johnson syndrome, haemolytic anaemia and vasculitis. Vasculitis can actually lead to atherosclerosis due to inflammation causing endothelial dysfunction.
Incredibly, with all the side effects associated with statins, Big Pharma are now encouraging people to combine statins with another cholesterol-lowering, injectable drug, Inclisiran. Inclisiran users can expect very common side effects (above 10%) such as liver problems and diabetes and, common side-effects (1-10%) such as angina, muscle pain, urinary tract infections, bronchitis and difficulty moving.
Summary
With the cholesterol theory of heart disease, the medical profession has misinterpreted a symptom for a cause. By perpetuating the myth, they have created a multi-billion industry to supply a drug, that not only doesn’t work but actually causes manifold illnesses, including heart problems. Moreover, even if you subscribe to the cholesterol theory, studies have shown that if you are over 50 years old, low levels of cholesterol have no beneficial effect and can even be dangerous and yet the average age for someone starting a course of statins is 62.
More likely causes of heart disease have been ignored because the treatment for those do not require any medical intervention but simply involves ensuring one avoids stress and has enough vitamins. There is, of course, no money to be made in that. In addition, there is now a patent to use statins as adjuvants in vaccines so there will be even more damage done. As always with Big Pharma, profit comes before health.








They have to know all this stuff. Demons. I think heart disease is caused by sugar. It causes inflammation. The body makes LDL to sooth inflammation. It's like saying we have to get rid of fire trucks because every time there's a fire, they're all over. But the ones at the top know. Not the doctors though.