The Dark Side of Antibiotics - Part 2
(The dangers they pose to your mental health)
Most people are now aware that the overuse of antibiotics has created dangerous antibiotic- resistant strains of bacteria or ‘superbugs’. Some people may even be aware of the serious physical, adverse reactions that antibiotics can cause– e.g. kidney and liver disease, colitis, Clostridium difficile, deafness and severe allergic reactions such as toxic epidermal necrolysis and anaphylaxis. However, how many people are aware that antibiotics can severely affect your mental health?
The link between antibiotics and psychiatric illnesses has been known for some time but is rarely mentioned in the media or highlighted by the mainstream medical establishment. An article twenty years ago in the Harvard Review of Psychiatry mentions antibiotics as causative agents of depression, panic attacks, delirium and psychosis.
In fact, the word ‘antibiomania’ has been coined to describe the psychotic symptoms associated with antibiotic use. Hoigne’s syndrome is a similar condition but relates to the symptoms of delusions and hallucinations suffered by some patients after receiving penicillin by injection. The Journal of Autoimmunity discovered 247 cases in medical literature where patients suffered auditory and visual hallucinations, confusion, anxiety and fear of death after being administered the drug, with five patients actually dying.
A case of antibiomania is examined in, ‘Case Reports in Psychiatry’. After the patient was started on a course of antibiotics, she started showing signs of -
‘Paranoia, anxiety, excessive fear, olfactory, visual and auditory hallucinations, religious utterances, nightmares, and a complete lack of sleep, approximately 24-48 hours after starting antibiotic treatment. Based on her family's report, she was apprehensive about her well-being and repeatedly asked if she was going to die. She did not sleep or eat for 3 days. She resisted seeking medical care as she felt convinced that God will cure her. ‘
Another side effect of Hoigne’s syndrome is psychomotor agitation, which involves repetitive movements linked to mania or anxiety. One of the treatments for this is the use of benzodiazepines. Disturbingly, the side effects of these drugs include agitation, hallucinations, aggression, psychosis, feeling out of touch with reality and suicidal thoughts. It is easy to see a scenario where someone goes to the doctor with antibiotic-induced mental issues, is given benzodiazepines, develops further psychotic symptoms and ends up in a psychiatric ward or on anti-psychotic medication for life.
It is interesting to note, therefore, that a study carried out by John Hopkins University stated that, of those people admitted into hospital with mania, there were five times more patients using antibiotics than not using them.
In some cases, the adverse effects certain antibiotics have on mental health have even been listed in the drug’s insert packaging. For example, in addition to the many serious physical side effects listed for the fluoroquinolone antibiotic, Levaquin, the insert also mentions the following effects, which can occur after just one dose –
“Confusion, hallucinations, paranoia, depression, nightmares, insomnia, and, rarely, suicidal thoughts or acts.”
Another antibiotic, Clarithromycin, part of the macrolide family of drugs, has listed side effects such as -
“Confusion about identity, place and time, feeling of unreality, feelings that others are watching or controlling your behaviour, feelings that others can hear your thoughts and feeling, seeing and hearing things that are not there.”
However, the detrimental mental effects are not just limited to these two classes of antibiotics. An article by the American Academy of Neurology noted mental issues,such as delusions and hallucinations,associated with 54 different antibiotics across 12 different classes of the drug.
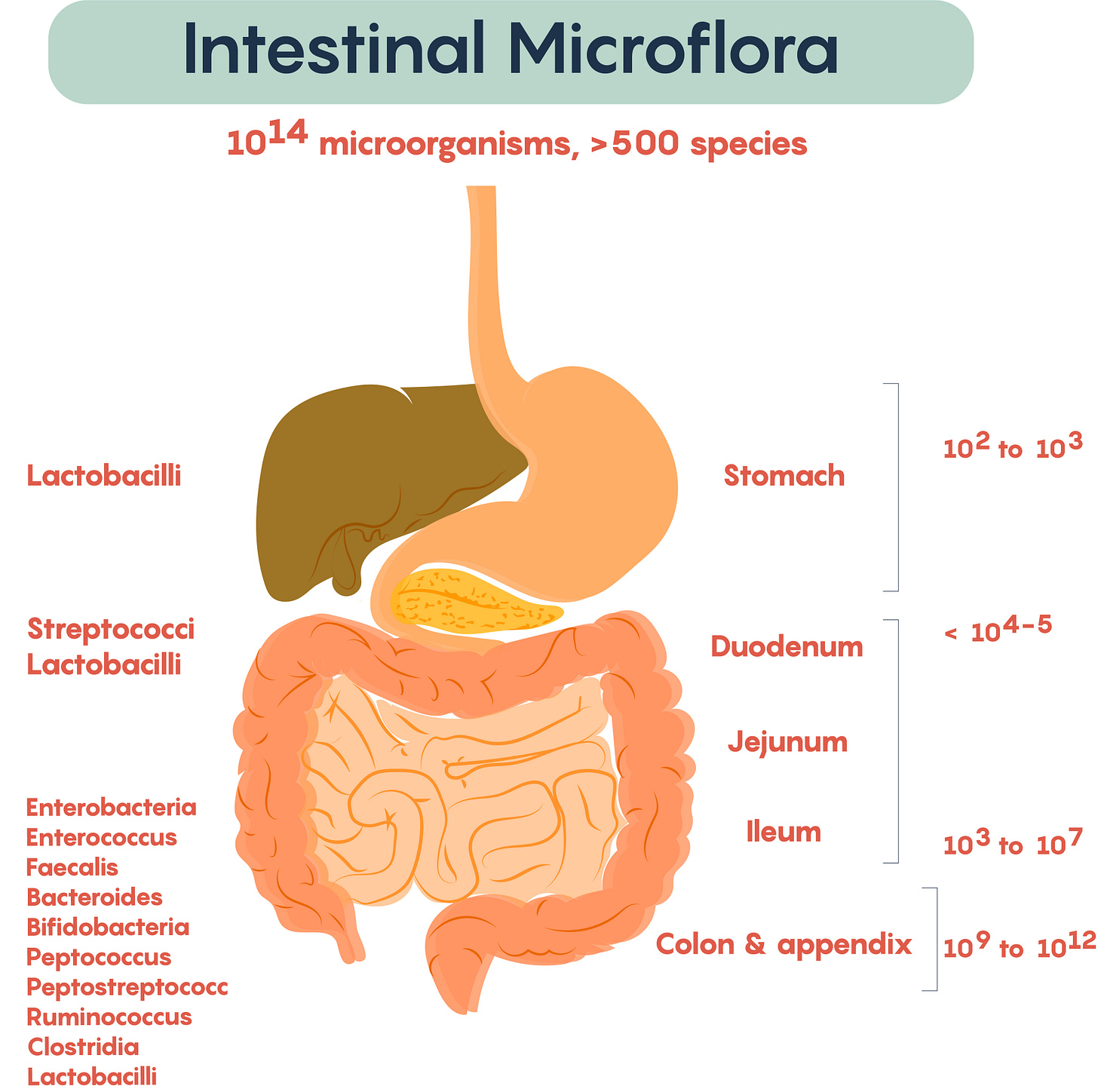
The Importance of the Microbiome
The fact that antibiotics may interfere with brain function shouldn’t come as a surprise. The drugs decimate the gut flora and it is now established that the health of the microbiome and diversity of bacterial colonies that comprise it, can have an impact on the brain.
It has also been discovered that certain bacterial species in the gut create mood altering chemicals. Bacillus bacteria, for example, create norepinephrine – a hormone and neurotransmitter which increases anxiety and restlessness but also promotes vigilance and helps with memory retrieval. Bacillis also produces dopamine which, in excess has been linked to bi-polar disease and at very low levels has been associated with schizophrenia.
Serotonin or 5-hydroxytryptamine (5-HT), is a neurotransmitter that affects mood, sleep, memory and arousal. However, 90% of serotonin is produced by the enterochromaffin cells in the gastrointestinal tract and this is only possible due to the actions of certain species of spore forming bacteria.
Gamma-Amino Butyric acid (GABA), an amino acid which acts as a neurotransmitter in the brain, inhibits nerve impulses, preventing anxiety and panic attacks. It has been shown that bifidobacteria and lactobacillus can both produce GABA.
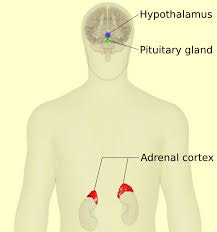
Recent research has highlighted the importance of what is known as the gut-brain axis, which is a two-way communication system between the gut and the central nervous system. Gut bacteria are an essential element of this communication pathway as they help regulate the Hypothalamic-Pituitary-Adrenal (HPA)axis which is involved in the stress response. HPA dysfunction is associated with post traumatic stress disorder, depression and borderline personality disorder.
The hypothalamus is part of the brain that sends messages out to the pituitary and the adrenal glands both of which then release a number of stress-related hormones. The type and number of bacterial colonies can affect how the HPA operates. The mechanisms by which this occurs are complex but according to a study in the Journal of Physiology –
“There is now overwhelming evidence that several cytokine families, especially interleukin-1, increase the secretory activity of the HPA axis; hence, it is reasonable to suppose that endotoxin and/or peptidoglycan, components of the bacterial cell wall, stimulate immune cells within the gut or elsewhere to release these cytokines, which consequently influence the parts of the CNS involved in the regulation of the HPA axis response.”
To emphasize the importance of gut bacteria in the regulation of the HPA axis and their effects an animal’s response to stress, a study was carried out on mice bred to be germ free. The results proved that the mice exhibited elevated Hypothalamic-Pituitary-Adrenal axis activity when faced with only minor stressors.
It has also been established that certain individuals display hypersensitive HPA axis activity and that this occurs due to early childhood trauma causing excessive stress. One of the major effects of excessive stress is an alteration to the gut flora in the microbiome, which, of course, is exactly what happens with the use of antibiotics.It is now being suggested that the health of the microbiota is the major factor influencing whether someone that has suffered a traumatic event will go on to suffer Post Traumatic Stress Disorder.
An article in the Canadian Journal of Psychiatry states –
“Recent experimental and clinical data converge on the hypothesis that imbalanced gut microbiota in early life may have long-lasting immune and other physiologic effects that make individuals more susceptible to develop PTSD after a traumatic event and contribute to the disorder.”
However, mental health problems can occur even earlier. Research has now established a link between gut dysbiosis in pregnancy and detrimental neural development, with particular focus on antibiotics as the cause of the microbial imbalance. As antibiotics comprise 80% of all medication prescribed to pregnant mothers, this should be of serious concern. A report in the Biomed Central Journal concurs by stating -
“We believe that the issue of antibiotics during pregnancy is one of the greatest challenges of human microbiome research and certainly deserves increased focus in the form of observational and interventional studies to unravel the role of these drugs in human development.”
Another known cause of mental health disorders is inflammation which has been linked to depression, anxiety, autism, dementia, and schizophrenia. The balance of gut microbes is important in this respect because certain bacteria, such as lactobacillus and bifidobacterium, inhibit the pro-inflammatory response. If colonies of these types of bacteria are significantly reduced by the use of antibiotics, the body’s ability to counter inflammation will be greatly reduced.
Leaky Gut, Candida and Psychiatric Disorders
Another intestinal condition that affects mental health is leaky gut syndrome. One of the main causes of this is an overgrowth of candida. Candida is an opportune fungus that can overwhelm the gut in the absence of other bacteria. It irritates the gut and the filamentous hyphae of the fungus penetrate the wall of the intestines leading to leaky gut syndrome.
Once again, antibiotics are the main culprits. According to Dr Jeffrey McCombs -
“Nothing else is guaranteed to create a systemic candida fungal infection in the body as fast, or as effectively as antibiotics. Nothing else but antibiotics cause systemic fungal candida infections on a routine basis for hundreds of millions of people worldwide.”
Mental health related symptoms associated with candidiasis are depression, seizures, confusion, mania, ADHD, autism, poor attention span, and learning difficulties. One of the mechanisms proposed for how candida affects the brain is via the production of acetaldehyde. This is a toxic, waste product created by the yeast. When it reacts with dopamine it can lead to depression, anxiety, and problems with concentration. In addition to this, acetaldehyde affects brain function in other ways. It restricts red blood cells’ ability to carry oxygen to the brain and inhibits the production of microtubules which are necessary to provide structure to nerve cells. It also causes a deficiency of vitamin B1which can lead to an illness called Wernicke-Korsakoff syndrome the symptoms of which are mental confusion, and poor memory.
Antibiotics, Pyroluria and Mental Illness
A further possible mechanism how dysbiosis may affect mental health is highlighted by the illness pyroluria. Hydroxyhemopyrrolin-2-one (HPL) is created in the production of the iron-containing compound heme. Over production of HPL can result in the body’s inability to utilise zinc and B6. Symptoms of this illness include delusions, paranoia, hallucinations, fearfulness, emotional instability and inability to think clearly.
Zinc and vitamin B6 are essential for production of neurotransmitters such as serotonin, melatonin and GABA which is why is why this illness can cause the same symptoms associated with so many mental disorders.
Pyroluria is usually a genetic disorder but can be caused by excessive use of antibiotics
Gut Dysbiosis and Autism
Recent research has linked autism to gut dysbiosis. An article in Bioessays, a journal on cellular and molecular biology,states –
“Alteration in the composition and metabolic products of the gut microbiome has long been implicated as a possible causative mechanism contributing to ASD pathophysiology.”
The Journal of Medical Microbiology also notes the link between the disruption of microbiota and autism and highlights a study which showed children with autism had higher levels of the pathogenic bacteria Clostridium histolyticum than non-autistic children. Clostridium tetani has also been found to be more prevalent in autistic children and has been linked to antibiotic use.
A particular aromatic compound, P cresol has been found to be elevated in children with autism. P cresol is toxic and is produced by the bacteria Clostridium difficile. It inhibits the enzyme, dopamine-beta-hydroxylase which converts dopamine to norepinephrine and can therefore lead to the onset of the symptoms of autism. A Clostridium difficile infection is nearly always caused by the use of antibiotics.
Antibiotics and Covid
Although covid was allegedly a virus, many patients were given antibiotics and the majority of those antibiotics were beta-lactams, which include penicillins. As we have seen, penicillin can cause Hoigne’s syndrome with its associated symptoms including delirium and psychomotor agitation. One of the medications used to treat this in covid patients was the drug aripiprazole. Incredibly, the side effects of this drug include anxiousness, restlessness and strange movements – the very symptoms of psychomotor agitation – so the patient’s agitated state would only increase.
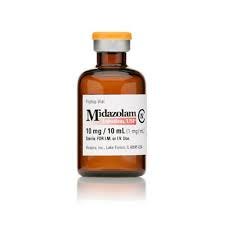
According to NHS official recommendations, patients suffering from anxiety and delirium should be given up to 5 mg of midazolam. However, according to the drug website, Drugs.com, the maximum dosage for light sedation is 2.5mg. And what are the side effects of midazolam? Restlessness, anxiety and irritability and trouble breathing.
So, we have a scenario whereby a patient diagnosed with covid , who could be on a course of antibiotics or receives antibiotics when they are hospitalised, becomes agitated due the antibiotics, is given drugs which exacerbate the problem, is then given midazolam which makes it worse still. The midazolam dose is therefore increased which results in supressed breathing resulting in them being put on a ventilator and subsequently dying because, as we now know, there is an extremely high death rate of ventilated patients.
How many patients died in this way during the covid scam? How many people died due to being diagnosed as being infected by a non-existent virus and then given antibiotics they didn’t need?
Treatment
If gut dysbiosis is the root cause of many psychiatric disorders, then there is potentially a simple solution – prebiotics and probiotics. Indeed, many scientists involved in the study of the microbiome are suggesting this as the way forward to re-balance the gut. Others are directly promoting the idea of using prebiotics and probiotics to alleviate the symptoms of mental disorders.
An article in the journal, Psychopharmacology, notes a study where the prebiotics, fructooligosaccharides and galactooligosaccharides proved to be natural anxiolytics, reducing anxiety and stress in a number of human test participants. Another article in, Nature, quoted a study where mice showing symptoms of autism were shown to have low levels of bacteroides fragilis. When this species of bacteria was increased the symptoms ceased. In a further study where the bacteria strains, Lactobacillus acidophilus Lactobacillus casei and Bifidobacterium were given to volunteers with depression, the test subjects reported a beneficial effect and a reduction in their symptoms.
Conclusion
This relatively recent area of research into the microbiome, is at last changing our perspective on the role of bacteria in our lives. Instead of seeing them as the enemy to be defeated at all costs, they are now being viewed by a new generation of scientists as essential for our physical and mental health. By indiscriminately using antibiotics to decimate them we are ultimately only damaging ourselves.
Perhaps we may even get to a point where a new protocol is implemented when someone shows symptoms of having a mental illness. Instead of immediately prescribing them extremely dangerous antipsychotic drugs, perhaps the doctors will establish if they are currently, or have recently been, on a course of antibiotics, test to see what types of bacteria are present or absent, and then prescribe probiotics to rectify the problem. Maybe, then we will start to see a vast improvement in people’s mental health.